Your new post is loading...

|
Scooped by
Juan Lama
|
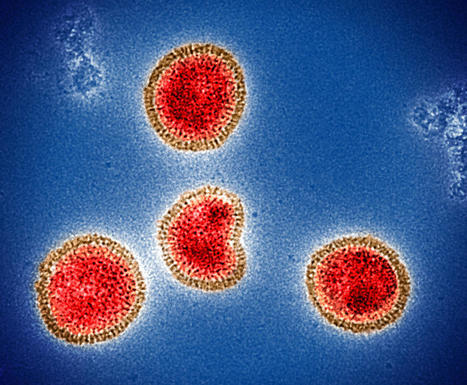
Researchers found associations between certain viral illnesses and the risk of Alzheimer’s and other neurodegenerative diseases. Neurodegenerative diseases can damage different parts of the nervous system, including the brain. This may lead to problems with thinking, memory, and/or movement. Examples include Alzheimer’s disease (AD), multiple sclerosis (MS), and Parkinson’s disease (PD). These diseases tend to happen late in life. There are few effective treatments. Previous findings have suggested that viruses may play a role in certain neurodegenerative diseases. For example, a recent study found a link between Epstein-Barr virus infection and the risk of MS. There are also concerns about cognitive impacts from SARS-CoV-2, the virus that causes COVID-19. A research team led by Drs. Mike Nalls, Kristin Levine, and Hampton Leonard of NIH's Center for Alzheimer’s and Related Dementias examined links between viruses and neurodegenerative disease more generally. To do so, they analyzed data from the FinnGen project. This is a repository of biomedical data, or biobank, from more than 300,000 people in Finland. The team searched the biobank for people who had been diagnosed with one of six different conditions: AD, amyotrophic lateral sclerosis (ALS), generalized dementia, vascular dementia, PD, and MS. They then checked how many had been hospitalized for a viral illness before. To confirm their findings, they looked for the same associations in the UK Biobank, which contains data from almost 500,000 people in the United Kingdom. Results appeared in Neuron on January 19, 2023. The researchers found 45 associations between viruses and neurodegenerative diseases in FinnGen. Of these, 22 also appeared in the UK Biobank. The strongest association was between viral encephalitis—brain inflammation caused by a virus—and AD. A person with viral encephalitis in the FinnGen database was 30 times as likely to be diagnosed with AD as someone without encephalitis. Results were similar in the UK Biobank; people with viral encephalitis were 22 times as likely to develop AD as those without. The team also found, in FinnGen, the association between Epstein-Barr virus and MS that was described before. The association wasn’t seen in the UK Biobank, but this may reflect how the different biobanks use hospital diagnostic codes; Epstein-Barr viruses are common and so often not noted. Influenza with pneumonia was associated with all the neurodegenerative diseases except MS. The researchers only included cases of influenza severe enough to need hospitalization in the study. Thus, these associations only apply to the most severe cases of influenza. FinnGen contains data on the same people over time. The team used this to examine how the associations depended on the time since infection. They found that some viral infections were associated with increased risk of neurodegenerative disease as much as 15 years later. The researchers note that vaccines exist for some of the viruses they identified. These include influenza, varicella-zoster (which causes chickenpox and shingles), and certain pneumonia-causing viruses. Vaccination might thus reduce some of the risk of the conditions they examined. “The results of this study provide researchers with several new critical pieces of the neurodegenerative disorder puzzle,” Nalls says. “In the future, we plan to use the latest data science tools to not only find more pieces but also help researchers understand how those pieces, including genes and other risk factors, fit together.”

|
Scooped by
Juan Lama
|
A recent study of more than 6 million people 65 and older found that seniors who had Covid-19 had a substantially higher risk of being diagnosed with Alzheimer's disease within a year. The study does not show that Covid-19 causes Alzheimer's, but it adds to the growing body of research drawing links between coronavirus infection and cognitive function. In the Alzheimer's disease brain, the pathology starts to build up about 20 years before the symptoms begin," said Dr. David Holtzman, a neurologist who leads a research lab focused on Alzheimer's disease at the Washington University School of Medicine in St. Louis. People would have to be followed for decades after a Covid-19 infection to prove it as a cause, he said. Instead, a Covid-19 infection could cause inflammation that may exacerbate changes that are already happening in the brain, experts say. "The brain has its own immune response to the pathology that's involved in [Alzheimer's] disease progressing," said Holtzman, who was not part of the new study. "When there are other things that cause inflammation that are in the body that can affect the brain, likely what happens is that can even amplify the process that's already going on." Other viruses can cause similar inflammation, experts say. Covid "is another one of the many dozen potential risk factors that I talked about with my patients," said Dr. Richard Isaacson, a neurologist and director of Florida Atlantic Unviersity's Center for Brain Health. He also was not involved in the new study but is a researcher focused on risk prevention for Alzheimer's disease. "I tell people to get a shingles vaccine. I tell people to get their annual flu and Pneumovax," and to exercise and eat a brain-healthy diet. Still, "when there's smoke, there's fire at some point," he said. "I really believe that this is something to at least pay attention to." The latest study, published last week in the Journal of Alzheimer's Disease, found that there were about seven new diagnoses of Alzheimer's disease for every 1,000 seniors who had a documented case of Covid-19 in the past year, compared with about five new diagnoses for every 1,000 who did not. Heather Snyder, vice president of medical and scientific relations at the Alzheimer's Association, notes that broader implications of the pandemic could have played into the study's findings. "The pandemic presented serious delays for individuals seeking out medical diagnoses like Alzheimer's, meaning these results could be driven by those who already had Alzheimer's when they were infected but had not yet sought out a formal diagnosis," she said. The study authors, along with Snyder and other experts, also identify this work as a call for more research on the underlying mechanisms of Alzheimer's disease that might explain the association. In the new study, the diagnosis of Alzheimer's was "mostly tentative," said Dr. Eliezer Masliah, director of the Division of Neuroscience at the National Institutes of Health's National Institute on Aging. Masliah, who was not involved in the study, said that there's evidence that Covid-19 might "trigger cognitive impairment," but there are new ways to confirm the link to Alzheimer's specifically. One next step would be to follow people at risk for Alzheimer's after a Covid-19 infection long-term to track biomarkers found in the blood and brain scans. "In the next couple of years, we're going to have a lot of very important information," Masliah said. And it's an "extremely important problem" to watch, given the scale of disease. "Imagine how many millions of people over the age of 60 or 65, like myself, have had Covid. Say 5% of them or 10% of them or even 1% of them are at risk," he said. "Wow. We're looking at a lot of people in the next few years that might add to the already very large epidemic of Alzheimer's disease that we have." About 6.5 million people over the age of 65 are living with Alzheimer's, according to estimates from the Alzheimer's Association. And it was the seventh leading cause of death in the US in 2020, according to data from the US Centers for Disease Control and Prevention. "Alzheimer's disease is a serious and challenging disease, and we thought we had turned some of the tide on it by reducing general risk factors such as hypertension, heart disease, obesity and a sedentary lifestyle," said Dr. Pamela Davis, a research professor at Case Western Reserve University and co-author of the new study. "Now, so many people in the US have had Covid, and the long-term consequences of Covid are still emerging. It is important to continue to monitor the impact of this disease on future disability."
|

|
Scooped by
Juan Lama
|
Clinical outcomes of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection are highly heterogeneous, ranging from asymptomatic infection to lethal coronavirus disease 2019 (COVID-19). The factors underlying this heterogeneity remain insufficiently understood. Genetic association studies have suggested that genetic variants contribute to the heterogeneity of COVID-19 outcomes, but the underlying potential causal mechanisms are insufficiently understood. Here we show that common variants of the Apolipoprotein E (APOE) gene, homozygous in approximately 3% of the world’s population1 and associated with Alzheimer’s disease, atherosclerosis and anti-tumor immunity2–5, impact COVID-19 outcome in a mouse model that recapitulates increased susceptibility conferred by male sex and advanced age. Mice bearing the APOE2 or APOE4 variant exhibited rapid disease progression and poor survival outcomes relative to mice bearing the most prevalent APOE3 allele. APOE2 and APOE4 mice exhibited increased viral loads as well as suppressed adaptive immune responses early after infection. In vitro assays demonstrated increased infection in the presence of APOE2 and APOE4 relative to APOE3, indicating that differential outcomes are mediated by differential effects of APOE variants on both viral infection and antiviral immunity. Consistent with these in vivo findings in mice, APOE genotype was associated with survival in SARS-CoV-2 infected patients in the UK Biobank (candidate variant analysis, P = 2.6×10-7). Our findings suggest APOE genotype to partially explain the heterogeneity of COVID-19 outcomes and warrant prospective studies to assess APOE genotyping as a means of identifying patients at high risk for adverse outcomes. Published in Nature (Sept. 21, 2022): https://doi.org/10.1038/s41586-022-05344-2
|



 Your new post is loading...
Your new post is loading...