Your new post is loading...

|
Scooped by
Juan Lama
|
Obesity is associated with an increased risk of severe Coronavirus Disease 2019 (COVID-19) infection and mortality. COVID-19 vaccines reduce the risk of serious COVID-19 outcomes; however, their effectiveness in people with obesity is incompletely understood. We studied the relationship among body mass index (BMI), hospitalization and mortality due to COVID-19 among 3.6 million people in Scotland using the Early Pandemic Evaluation and Enhanced Surveillance of COVID-19 (EAVE II) surveillance platform. We found that vaccinated individuals with severe obesity (BMI > 40 kg/m2) were 76% more likely to experience hospitalization or death from COVID-19 (adjusted rate ratio of 1.76 (95% confidence interval (CI), 1.60–1.94). We also conducted a prospective longitudinal study of a cohort of 28 individuals with severe obesity compared to 41 control individuals with normal BMI (BMI 18.5–24.9 kg/m2). We found that 55% of individuals with severe obesity had unquantifiable titers of neutralizing antibody against authentic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus compared to 12% of individuals with normal BMI (P = 0.0003) 6 months after their second vaccine dose. Furthermore, we observed that, for individuals with severe obesity, at any given anti-spike and anti-receptor-binding domain (RBD) antibody level, neutralizing capacity was lower than that of individuals with a normal BMI. Neutralizing capacity was restored by a third dose of vaccine but again declined more rapidly in people with severe obesity. We demonstrate that waning of COVID-19 vaccine-induced humoral immunity is accelerated in individuals with severe obesity. As obesity is associated with increased hospitalization and mortality from breakthrough infections, our findings have implications for vaccine prioritization policies. Epidemiological analyses coupled with immunological phenotyping suggest that humoral immunity induced by COVID-19 vaccines wanes more rapidly in individuals with severe obesity compared to individuals with a BMI within the normal range. Published in Nature Medicine (May 11, 2023): https://doi.org/10.1038/s41591-023-02343-2

|
Scooped by
Juan Lama
|
Caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), coronavirus disease 2019 (COVID-19) has diverse clinical manifestations, which is the main feature of the disease, and the fundamental reason is the different immune responses in different bodies among the population. The damage mechanisms of critical illness by SARS-CoV-2 and its variants, such as hyperinflammatory response, a double-edged function of type I interferon, and hyperactivation of the complement system, are the same as other critical illnesses. Targeting specific immune damage mechanisms of COVID-19, we scored the first to put forward that the responses of T cells induced by acute virus infection result in “acute T-cell exhaustion” in elderly patients, which is not only the peripheral exhaustion with quantity reduction and dysfunction of T cells but also the central exhaustion that central immune organs lost immune homeostasis over peripheral immune organs, whereas the increased thymic output could alleviate the severity and reduce the mortality of the disease with the help of medication. We discovered that immune responses raised by SARS-CoV-2 could also attack secondary lymphoid organs, such as the spleen, lymphoid nodes, and kidneys, in addition to the lung, which we generally recognize. Integrated with the knowledge of mechanisms of immune protection, we developed a coronavirus antigen diagnostic kit and therapeutic monoclonal antibody. In the future, we will further investigate the mechanisms of immune damage and protection raised by coronavirus infection to provide more scientific strategies for developing new vaccines and immunotherapies. Published in Frontiers in Immunology (March 7, 2023): https://doi.org/10.3389/fimmu.2023.1130398

|
Scooped by
Juan Lama
|
New studies are boosting assessments that immunity to COVID-19 lasts at least 6-8 months after recovery from the disease. Research published in Science Immunology this week examined 25 patients recovering from the illness. Though antibodies — the immune system proteins that attack virus particles — began dropping in blood samples some 20 days after symptoms appeared, memory B cells that produce antibodies continued to rise in the blood for 150 days and remained high until the 240-day point. This signals subjects’ bodies were primed to fight off the virus for some eight months. Meanwhile, researchers in two other studies found that people who made antibodies to the coronavirus were much less likely to test positive again for up to six months and maybe longer The results bode well for vaccines, which provoke the immune system to make antibodies. A study published Wednesday by the New England Journal of Medicine involved more than 12,500 health workers at Oxford University Hospitals in the United Kingdom. Among the 1,265 who had coronavirus antibodies at the outset, only two had positive results on tests to detect active infection in the following six months and neither developed symptoms. That contrasts with the 11,364 workers who initially did not have antibodies; 223 of them tested positive for infection in the roughly six months that followed. A third study by the National Cancer Institute study involved more than 3 million people who had antibody tests from two private labs in the United States. Only 0.3% of those who initially had antibodies later tested positive for the coronavirus, compared with 3% of those who lacked such antibodies. The results showed that people with antibodies from natural infections were “at much lower risk… on the order of the same kind of protection you’d get from an effective vaccine,” of getting the virus again, said Dr. Ned Sharpless, director of the US National Cancer Institute. “It’s very, very rare” to get reinfected, he said. The institute’s study had nothing to do with cancer — many federal researchers have shifted to coronavirus work because of the pandemic. “It’s very gratifying” to see that the Oxford researchers saw the same risk reduction — 10 times less likely to have a second infection if antibodies were present, Sharpless said. His institute’s report was posted on a website scientists use to share research and is under review at a major medical journal. The findings are “not a surprise … but it’s really reassuring because it tells people that immunity to the virus is common,” said Joshua Wolf, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis who had no role in either study. “We don’t know how long-lasting this immunity is,” Wolf added. Cases of people getting COVID-19 more than once have been confirmed, so “people still need to protect themselves and others by preventing reinfection.” Findings Published in Science Immunology (Dec. 22, 2020): https://doi.org/10.1126/sciimmunol.abf8891 NEJM (DEc. 23, 2020): https://doi.org/10.1056/NEJMoa2034545

|
Scooped by
Juan Lama
|
Sanofi had previously projected it could produce 100 million doses of vaccine in 2020, and 1 billion doses in 2021. One of the world’s leading vaccine manufacturers has suffered a major setback in its work to produce a Covid-19 vaccine. The problem will push the timeline for deployment of Sanofi Pasteur’s vaccine — if it is approved — from the first half of 2021 into the second half of the year, the company said Friday. The news is not just disappointing for Sanofi and its development partner, GlaxoSmithKline, which is providing an adjuvant used in the vaccine. The companies have contracts with multiple countries, including the United States and Britain, as well as the European Union. Sanofi had hoped to start a Phase 3 trial of the vaccine this month and had projected it could produce 100 million doses of vaccine in 2020, and 1 billion doses in 2021. The problem relates to inadequate results in older adults in Sanofi’s Phase 1/2 trial, which the company traced back to an inadequate formulation of their vaccine, Su-Peing Ng, global medical head for Sanofi Vaccines, told STAT in an interview. Ng said both Sanofi and GSK are committed to continuing work on the vaccine, and plan to begin a Phase 2b trial in February. “We’re disappointed that there is a delay,” she said. “I think, though, that we’re encouraged that we have enough information, enough of the results from preclinical and clinical [studies] to tell us that we have a path forward. We need to optimize this formulation.” In effect, participants in the trial received too little vaccine. While the too-small dose generated adequate levels of neutralizing antibodies in adults aged 18 to 49 in the trial, adults 60 and older generated lower levels of neutralizing antibodies than are seen in the blood of people who have recovered from Covid-19 infection, Ng said. Perplexed by the findings, the company set out to figure out why the vaccine underperformed. It discovered two commercial reagents used to measure how much antigen — active vaccine — was included in each dose were giving false readings. In fact, Ng said, the concentration of the antigen “was insufficient.” A revised formulation, tested recently in non-human primates, showed the vaccine prevented damage in the lungs, which is what triggers severe Covid disease in people, and led to rapid clearance of the virus. The vaccine’s path will be more challenging because of this delay; the Covid vaccine landscape is changing daily and placebo-controlled trials may not be feasible for much longer, with the first vaccines soon to be deployed. If people know they may soon have access to an authorized vaccine, there is less motivation to enroll in a trial where they might get a placebo. Sanofi knows this and is proposing to the Food and Drug Administration that its Phase 2b trial compare its vaccine to one that is already authorized, not a placebo. “To continue to provide confidence that we’re going to have a vaccine that meets the expected standard of care, we propose the comparison with an authorized Covid-19 vaccine instead of placebo control,” Ng said. That would set a very high bar for the Sanofi vaccine. Pfizer and Moderna, the front-runners in the vaccine race, have reported vaccine efficacy of about 95% in their Phase 3 trials. If the Sanofi vaccine doesn’t reach that level of efficacy, can it be brought to market, STAT asked Ng. “That will be up to the regulators,” she said, adding that “for the public to be confident in the choice of a vaccine, it would have to be pretty close to what’s been established now. The Sanofi vaccine would have one advantage compared to the Pfizer and Moderna vaccines: It wouldn’t require ultracold storage and could instead be kept in standard refrigerators, making it easier to distribute Pfizer and Moderna are poised to receive emergency use authorizations from the FDA this month — an FDA advisory panel endorsed the Pfizer shot on Thursday — and vaccine rollout in the United States is expected to begin within days of the FDA’s green light. The Phase 3 trial for Johnson & Johnson’s vaccine — the only one-dose vaccine currently in clinical trials in the U.S. — is about to finish enrollment; if it is effective, it could get an EUA in the first quarter of 2021. The Sanofi vaccine is made with an approach the company uses for one of its flu vaccines, Flubok. That in theory is an advantage; the FDA knows how this vaccine system works. It’s called a recombinant protein vaccine, with the spike protein of the SARS-CoV-2 virus, which cases Covid-19, generated in insect cells. Sanofi is also developing a second vaccine, a messenger RNA vaccine, like the Pfizer and Moderna shots. For this project, it is collaborating with Translate Bio, a Lexington, Mass.-based biotech. Clinical trials for that vaccine have not yet begun.
|

|
Scooped by
Juan Lama
|
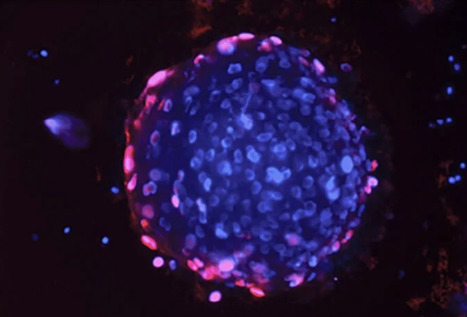
Aging, or senescent cells, which stop dividing but don’t die, can accumulate in the body over the years and fuel chronic inflammation that contributes to conditions such as cancer and degenerative disorders. In mice, eliminating senescent cells from aging tissues can restore tissue balance and lead to an increased healthy lifespan. Now a team led by investigators at Massachusetts General Hospital (MGH), a founding member of Mass General Brigham (MGB), has found that the immune response to a virus that is ubiquitously present in human tissues can detect and eliminate senescent cells in the skin. For the study, which is published in Cell, the scientists analyzed young and old human skin samples to learn more about the clearance of senescent cells in human tissue. The researchers found more senescent cells in the old skin compared with young skin samples. However, in the samples from old individuals, the number of senescent cells did not increase as individuals got progressively older, suggesting that some type of mechanism kicks in to keep them in check. Experiments suggested that once a person becomes elderly, certain immune cells called killer CD4+ T cells are responsible for keeping senescent cells from increasing. Indeed, higher numbers of killer CD4+ T cells in tissue samples were associated with reduced numbers of senescent cells in old skin. When they assessed how killer CD4+ T cells keep senescent cells in check, the researchers found that aging skin cells express a protein, or antigen, produced by human cytomegalovirus, a pervasive herpesvirus that establishes lifelong latent infection in most humans without any symptoms. By expressing this protein, senescent cells become targets for attack by killer CD4+ T cells. “Our study has revealed that immune responses to human cytomegalovirus contribute to maintaining the balance of aging organs,” says senior author Shawn Demehri, MD, PhD, director of the High Risk Skin Cancer Clinic at MGH and an associate professor of Dermatology at Harvard Medical School. “Most of us are infected with human cytomegalovirus, and our immune system has evolved to eliminate cells, including senescent cells, that upregulate the expression of cytomegalovirus antigens.” These findings, which highlight a beneficial function of viruses living in our body, could have a variety of clinical applications. “Our research enables a new therapeutic approach to eliminate aging cells by boosting the anti-viral immune response,” says Demehri. “We are interested in utilizing the immune response to cytomegalovirus as a therapy to eliminate senescent cells in diseases like cancer, fibrosis and degenerative diseases.” Demehri notes that the work may also lead to advances in cosmetic dermatology, for example in the development of new treatments to make skin look younger. Co-authors include Tatsuya Hasegawa, Tomonori Oka, Heehwa G. Son, Valeria S. Oliver-García, Marjan Azin, Thomas M. Eisenhaure, David J. Lieb, and Nir Hacohen. This study was supported by the Burroughs Wellcome Fund and Shiseido Co. Ltd. Study Published in Cell (March 30, 2023): https://doi.org/10.1016/j.cell.2023.02.033

|
Scooped by
Juan Lama
|
Cele et al. examine a SARS-CoV-2 infection persisting over 6 months, starting as ancestral virus but evolving various mutations found in Omicron and other variants. The evolved virus substantially but incompletely escaped BNT162b2-elicited immunity as well as neutralization by self-plasma and showed extensive escape from neutralization elicited by Delta infections. Characterizing SARS-CoV-2 evolution in specific geographies may help predict properties of variants coming from these regions. We mapped neutralization of a SARS-CoV-2 strain that evolved over 6 months from ancestral virus in a person with advanced HIV disease in South Africa, infected prior to emergence of the Beta and Delta variants. We longitudinally tracked the evolved virus and tested it against self-plasma and convalescent plasma from ancestral, Beta, and Delta infections. Early virus was similar to ancestral but evolved a multitude of mutations found in Omicron and other variants. It showed substantial but incomplete Pfizer BNT162b2 escape, weak neutralization by self-plasma, and despite pre-dating Delta, extensive escape of Delta infection-elicited neutralization. This example is consistent with the notion SARS-CoV-2 evolving in individual immune-compromised hosts, including those with advanced HIV disease, may gain immune escape of vaccines and enhanced escape of Delta immunity, with implications for vaccine breakthrough and reinfections. Published in Cell and Host Microbe (Jan. 13, 2022): https://doi.org/10.1016/j.chom.2022.01.005

|
Scooped by
Juan Lama
|
New research by scientists at the University of Chicago suggests a person's antibody response to influenza viruses is dramatically shaped by their pre-existing immunity, and that the quality of this response differs in individuals who are vaccinated or naturally infected. Their results highlight the importance of receiving the annual flu vaccine to induce the most protective immune response. The researchers found that most of the initial antibodies stimulated after both influenza infections and influenza vaccinations came from old B cells—a type of white blood cell that secretes antibodies—indicating the immune system's memory plays a major role in how the body responds early on to a viral infection. These antibodies displayed higher reactivity toward strains of influenza that circulated during an individual's childhood compared to more recent strains. The study, published December 10, 2020 in the journal Science Translational Medicine, provides those working on a universal influenza vaccine further understanding of how pre-existing immunity affects the development and performance of neutralizing and non-neutralizing antibodies following infection and vaccination. Any effective universal influenza vaccine will depend on scientists identifying 'conserved' parts of the influenza virus that do not mutate over time and that antibodies can target to prevent infection. "Most interestingly, we found that people who were actively sick with influenza had old antibodies that predominantly targeted parts of the virus that don't change—but those antibodies specifically targeted non-neutralizing sites," said Haley Dugan, co-first author of the study and a Ph.D. candidate in immunology. "When we tested these same antibodies in mice, they weren't able to protect them from being infected with influenza." In contrast, the researchers found that influenza vaccinations boost antibodies that tended to target conserved yet neutralizing regions of the virus, which suggests vaccinations can draw upon pre-existing immunity to prompt more protective responses. Vaccinated individuals also generated many antibodies that targeted new and mutated regions on the virus, suggesting these vaccine-induced antibodies are more adaptable. Immune system memory ensures a rapid and specific response to previously encountered pathogens. Vaccinations work by exposing the immune system to a small amount of virus, which causes B cells to develop a biological memory to the virus. If the body encounters the same virus later, the immune system is alerted to attack and eliminate the virus. But in order to be protected, the viral proteins of the infecting strain must typically match those of the strain used in the vaccine. The memory B cells are like keys that fit and bind to the locks—the viral proteins. These memory B cells can survive for decades, providing long-lasting protection from future infections. But if the virus mutates and is significantly different, the memory B cells can no longer recognize the viral proteins, potentially leading to infection. For this reason, the human body is pitted in an evolutionary arms race with the flu. Because influenza viruses rapidly evolve and mutate each season, our immune system has trouble recognizing the viral surface proteins on new influenza strains. As a result, our bodies often rely on old antibodies to fight new influenza strains; this is possible because some parts of the influenza virus that are critical to its structure or function do not change, remaining familiar to our immune system. Researchers now understand that specific structural and functional parts of the influenza virus that do not change are better for antibodies to target than others. Antibodies that bind to one of these neutralizing sites are able to prevent infection, while antibodies that target non-neutralizing sites often cannot. Scientists believe a person's age, history of exposure to the influenza virus and type of exposure—either through infection or vaccination—all shape whether their immune system antibodies target neutralizing or non-neutralizing sites on a virus. In the UChicago study, scientists sought to address a major knowledge gap: Which conserved viral sites are preferentially targeted following natural infection versus vaccination in people, and how does pre-existing immunity play a role in shaping the landscape of neutralizing and non-neutralizing antibodies? "For people who have caught the flu, their pre-existing immunity may make them susceptible to infection or increase the severity of their influenza symptoms if their antibodies are targeting 'bad' or non-neutralizing viral sites," said co-first author and Immunology postdoctoral fellow Jenna Guthmiller, Ph.D. By contrast, vaccination largely induces neutralizing and protective antibodies, old and new, highlighting the importance of receiving the seasonal influenza vaccine. "This study provides a major framework for understanding how pre-existing immunity shapes protective antibody responses to influenza in humans," said Patrick Wilson, Ph.D., a professor of immunology and lead author of the study. "We need more studies to determine whether the targeting of specific neutralizing and non-neutralizing viral sites directly impacts a person's likelihood of becoming ill." The researchers are now examining how early exposure to the influenza virus in children shapes their immune response later in life as a follow-up to this work. Cited Research Published in Science Translational Medicine (Dec. 9, 2020): https://doi.org/10.1126/scitranslmed.abd3601

|
Scooped by
Juan Lama
|
New research indicates that human immune system cells are storing information about the coronavirus so they can fight it off again. To the immune system, not all germs are equally memorable. But our body’s cells seem to be seriously studying up on the coronavirus. Scientists who have been monitoring immune responses to the virus are now starting to see encouraging signs of strong, lasting immunity, even in people who developed only mild symptoms of Covid-19, a flurry of new studies suggests. Disease-fighting antibodies, as well as immune cells called B cells and T cells that are capable of recognizing the virus, appear to persist months after infections have resolved — an encouraging echo of the body’s enduring response to other viruses. “Things are really working as they’re supposed to,” said Deepta Bhattacharya, an immunologist at the University of Arizona and an author on one of the new studies, which has not yet been peer-reviewed. Although researchers cannot forecast how long these immune responses will last, many experts consider the data a welcome indication that the body’s most studious cells are doing their job — and will have a good chance of fending off the coronavirus, faster and more fervently than before, if exposed to it again. “This is exactly what you would hope for,” said Marion Pepper, an immunologist at the University of Washington and an author on another of the new studies, which is currently under review at the journal Nature. “All the pieces are there to have a totally protective immune response.” Protection against reinfection cannot be fully confirmed until there is proof that most people who encounter the virus a second time are actually able to keep it at bay, Dr. Pepper said. But the findings could help quell recent concerns over the virus’s ability to dupe the immune system into amnesia, leaving people vulnerable to repeat bouts of disease. Researchers have yet to find unambiguous evidence that coronavirus reinfections are occurring, especially within the few months that the virus has been rippling through the human population. The prospect of immune memory “helps to explain that,” Dr. Pepper said. In discussions about immune responses to the coronavirus, much of the conversation has focused on antibodies — Y-shaped proteins that can latch onto the surfaces of pathogens and block them from infecting cells. But antibodies represent just one wing of a complex and coordinated squadron of immune soldiers, each with their own unique modes of attack. Viruses that have already invaded cells, for instance, are cloaked from antibodies, but are still vulnerable to killer T cells, which force infected cells to self-destruct. Another set of T cells, nicknamed “helpers,” can coax B cells to mature into antibody-making machines. (Yet another sector of the immune system assails pathogens within minutes of their arrival, while sending out signals called cytokines to mobilize forces from elsewhere in the body. Some evidence suggests that severe cases of Covid-19 may stem from this early process going awry.) Antibodies also come with an expiration date: Because they are inanimate proteins and not living cells, they can’t replenish themselves, and so disappear from the blood just weeks or months after they are produced. Hordes of antibodies appear shortly after a virus has breached the body’s barriers, then wane as the threat dissipates. Most of the B cells that produce these early antibodies die off as well. But even when not under siege, the body retains a battalion of longer-lived B cells that can churn out virus-fighting antibodies en masse, should they prove useful again. Some patrol the bloodstream, waiting to be triggered anew; others retreat into the bone marrow, generating small amounts of antibodies that are detectable years, sometimes decades, after an infection is over. Several studies, including those led by Dr. Bhattacharya and Dr. Pepper, have found antibodies capable of incapacitating the coronavirus lingering at low levels in the blood months after people have recovered from Covid-19. “The antibodies decline, but they settle in what looks like a stable nadir,” which is observable about three months after symptoms start, Dr. Bhattacharya said. “The response looks perfectly durable.”...
|



 Your new post is loading...
Your new post is loading...