Your new post is loading...

|
Scooped by
Juan Lama
|
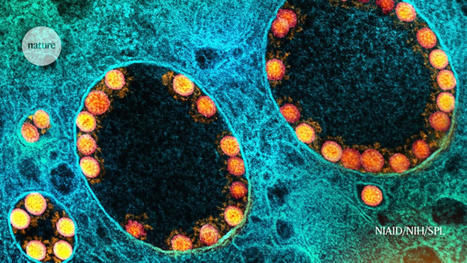
New results hint at how to perfect ‘mucosal’ vaccines, which are delivered up the nose or down the throat. Delivery of COVID vaccines directly to the lungs and nose can stop SARS-CoV-2 infections in their tracks, according to a trio of new studies in monkeys. The research offers a boost to the wave of ‘mucosal’ COVID-19 vaccines now in development — and provides clues about how they might be improved. Until now, there has been little evidence that mucosal vaccines, which are taken by nose or mouth, shield people against infection any better than existing COVID-19 jabs do. Even so, some countries have already approved such vaccines, and key trials are under way in the United States, with others set to start. Together, the studies show that how and where vaccines are delivered can have a profound effect on the immunity generated and the protection conferred. The latest results also raise hopes that mucosal vaccines that offer ‘sterilising’ immunity — complete blockage of infection — could become a reality. “These studies are showing you can get near sterilising immunity,” says Akiko Iwasaki, an immunologist at the Yale School of Medicine in New Haven, Connecticut. "It’s not complete science fiction to think about developing vaccines that would stop transmission and infection....

|
Scooped by
Juan Lama
|
Cells taken from patients at the time of diagnosis who later developed severe COVID-19 show a muted antiviral response, study finds. - Researchers studied cells collected by nasal swabs at the moment of diagnosis for both mild and severe COVID-19 patients
- Cells taken from patients who went on to develop severe disease had a muted antiviral response compared to those who went on to develop mild disease
- This suggests that it may be possible to develop early interventions that prevent severe COVID-19 from developing
- The team also identified infected host cells and pathways associated with protection against infection that may enable new therapeutic strategies for COVID-19 and other respiratory viral infections
Over the past 18 months, researchers have learned much about COVID-19 and its viral cause, SARS-CoV-2. They know how the virus enters the body, coming in through the nose and mouth and beginning its infection in the mucus layers of the nasal passageway. They know that infections that remain in the upper airway are likely to be mild or asymptomatic, while infections that progress down the airway to the lungs are much more severe and can lead to fatal disease. And they have identified common risk factors for severe disease, like age, gender, and obesity. But there are still many unanswered questions — such as when, and where, the course of severe COVID-19 is determined. Does the pathway to severe disease begin only after the body has failed to control mild disease, or could it start much earlier than that? Researchers at the Ragon Institute of MGH, MIT, and Harvard; the Broad Institute of MIT and Harvard; Boston Children’s Hospital (BCH); MIT; and the University of Mississippi Medical Center (UMMC) wondered whether this path towards severe disease could start much earlier than expected — perhaps even within the initial response created when the virus enters the nose. To test this, they studied cells taken from nasal swabs of patients at the time of their initial COVID-19 diagnosis, comparing patients who went on to develop mild COVID-19 to those who progressed into more severe disease and eventually required respiratory support. Their results showed that patients who went on to develop severe COVID-19 exhibited a much more muted antiviral response in the cells collected from those early swabs, compared to patients who had a mild course of disease. The paper appears in the journal Cell. “We wanted to understand if there were pronounced differences in samples taken early in the course of disease that were associated with different severities of COVID-19 as the disease progressed,” said co-senior author José Ordovás-Montañés, an associate member in the Klarman Cell Observatory at Broad and assistant professor at BCH and Harvard Medical School. “Our findings suggest that the course of severe COVID-19 may be determined by the body’s intrinsic antiviral response to initial infection, opening up new avenues for early interventions that could prevent severe disease.” To understand the early response to infection, Sarah Glover of the Division of Digestive Diseases at UMMC and her laboratory collected nasal swabs from 58 people. Thirty-five swabs came from COVID-19 patients, taken at the time of diagnosis, representing a variety of disease states from mild to severe. Seventeen swabs came from healthy volunteers and six came from patients with respiratory failure due to other causes. The team isolated individual cells from each sample and sequenced them, looking for RNA that would indicate what kind of proteins the cells were making — a proxy for understanding what a given cell is doing at the moment of collection. Cells use RNA as instructions to make proteins — tools, machinery, and building blocks used within and by the cell to perform different functions and respond to its environment. By studying the collection of RNA in a cell — its transcriptome — researchers understand how a cell is responding, at that particular moment in time, to environmental changes such as a viral infection. Researchers can even use the transcriptome to see if individual cells are infected by an RNA virus like SARS-CoV-2. Alex Shalek, co-senior author on the study, a member of the Ragon Institute of MGH, MIT, and Harvard, and institute member at Broad, specializes in studying the transcriptomes of individual cells. His lab has helped develop innovative approaches to sequence thousands of single cells from low-input clinical samples, like the nasal swab of COVID-19 patients, and uses the resulting data to create high-resolution pictures of the body’s orchestrated response to infection at the sample site. “Our single-cell sequencing approaches allow us to comprehensively study the body’s response to disease at a specific moment in time,” said Shalek, who is also an associate professor at MIT in the Institute for Medical Engineering & Science, the Department of Chemistry, and the Koch Institute for Integrative Cancer Research. “This gives us the ability to systematically explore features that differentiate one course of disease from another as well as cells that are infected from those that are not. We can then leverage this information to guide the development of more effective preventions and cures for COVID-19 and other viral infections.” Ordovás-Montañés’s lab studies inflammatory responses and their memory, specializing in those found in epithelial cells — the top layer of cells, like those that line your nasal passageways and are collected by nasal swabs. Working with the Shalek lab and that of Bruce Horwitz, a senior associate physician in the BCH Division of Emergency Medicine, the researchers interrogated how both epithelial and immune cells were responding to early COVID-19 infection from the single-cell transcriptome data. First, the team found that the antiviral response, driven by a family of proteins called interferons, was much more muted in patients who went on to develop severe COVID-19. Second, patients with severe COVID-19 had higher amounts of highly inflammatory macrophages, immune cells that contribute to high amounts of inflammation, often found in severe or fatal COVID-19. Since these samples were taken well before COVID-19 had reached its peak state of disease in the patients, both these findings indicate that the course of COVID-19 may be determined by the initial or very early response of the nasal epithelial and immune cells to the virus. The lack of strong initial antiviral response may allow the virus to spread more rapidly, increasing the chances that it can move from the upper to lower airways, while the recruitment of inflammatory immune cells could help drive the dangerous inflammation in severe disease. Finally, the team also identified infected host cells and pathways associated with protection against infection — cells and responses unique to patients that went on to develop a mild disease. These findings may allow researchers to discover new therapeutic strategies for COVID-19 and other respiratory viral infections. If, as the team’s evidence suggests, the early stages of infection can determine disease, it opens a path for scientists to develop early interventions that can help prevent severe COVID-19 from developing. The team’s work even identified potential markers of severe disease, genes that were expressed in mild COVID-19 but not in severe COVID-19. “Nearly all our severe COVID-19 samples lacked expression of several genes we would typically expect to see in an antiviral response,” said Carly Ziegler, a graduate student in the Health Science and Technology program at MIT and Harvard and one of the study’s co-first authors. “If further studies support our findings, we could use the same nasal swabs we use to diagnose COVID-19 to identity potentially severe cases before severe disease develops, creating an opportunity for effective early intervention.” Research Cited Published in Cell: https://www.cell.com/cell/pdf/S0092-8674(21)00882-5.pdf

|
Scooped by
Juan Lama
|
Scientists at Columbia University have developed a treatment that blocks the virus in the nose and lungs, is inexpensive and needs no refrigeration. A nasal spray that blocks the absorption of the SARS-CoV-2 virus has completely protected ferrets it was tested on, according to a small study released on Thursday by an international team of scientists. The study, which was limited to animals and has not yet been peer-reviewed, was assessed by several health experts at the request of The New York Times. If the spray, which the scientists described as nontoxic and stable, is proved to work in humans, it could provide a new way of fighting the pandemic. A daily spritz up the nose would act like a vaccine. “Having something new that works against the coronavirus is exciting,” said Dr. Arturo Casadevall, the chairman of immunology at the Johns Hopkins Bloomberg School of Public Health, who was not involved in the study. “I could imagine this being part of the arsenal.” The work has been underway for months by scientists from Columbia University Medical Center in New York, Erasmus Medical Center in the Netherlands and Cornell University in Ithaca, N.Y., The study was funded by the National Institutes of Health and the Columbia University Medical Center. The team would require additional funding to pursue clinical trials in humans. Dr. Anne Moscona, a pediatrician and microbiologist at Columbia and co-author of the study, said they had applied for a patent on the product, and she hoped Columbia University would approach the federal government’s Operation Warp Speed or large pharmaceutical companies that are seeking new ways to combat the coronavirus. The spray attacks the virus directly. It contains a lipopeptide, a cholesterol particle linked to a chain of amino acids, the building blocks of proteins. This particular lipopeptide exactly matches a stretch of amino acids in the spike protein of the virus, which the pathogen uses to attach to a human airway or lung cell. Before a virus can inject its RNA into a cell, the spike must effectively unzip, exposing two chains of amino acids, in order to fuse to the cell wall. As the spike zips back up to complete the process, the lipopeptide in the spray inserts itself, latching on to one of the spike’s amino acid chains and preventing the virus from attaching. “It is like you are zipping a zipper but you put another zipper inside, so the two sides cannot meet,” said Matteo Porotto, a microbiologist at Columbia University and one of the paper’s authors. The work was described in a paper posted to the preprint server bioRxiv Thursday morning, and has been submitted to the journal Science for peer review. Dr. Peter J. Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine, said the therapy looked “really promising.” “What I’d like to know now is how easy it is to scale production,” he said. In the study, the spray was given to six ferrets, which were then divided into pairs and placed in three cages. Into each cage also went two ferrets that had been given a placebo spray and one ferret that had been deliberately infected with SARS-CoV-2 a day or two earlier. Ferrets are used by scientists studying flu, SARS and other respiratory diseases because they can catch viruses through the nose much as humans do, although they also infect each other by contact with feces or by scratching and biting. After 24 hours together, none of the sprayed ferrets caught the disease; all the placebo-group ferrets did. “Virus replication was completely blocked,” the authors wrote... Study cited available at bioRxiv (Nov. 4, 2020): https://doi.org/10.1101/2020.11.04.361154

|
Scooped by
Juan Lama
|
Saliva Specimens to Detect SARS-CoV-2 Infection In this letter, the investigators report that saliva specimens and nasopharyngeal swab specimens had similar sensitivity in the detection of COVID-19. Rapid and accurate diagnostic tests are essential for controlling the ongoing Covid-19 pandemic. Although the current standard involves testing of nasopharyngeal swab specimens by quantitative reverse-transcriptase polymerase chain reaction (RT-qPCR) to detect SARS-CoV-2, saliva specimens may be an alternative diagnostic sample. Rigorous evaluation is needed to determine how saliva specimens compare with nasopharyngeal swab specimens with respect to sensitivity in detection of SARS-CoV-2 during the course of infection. A total of 70 inpatients with Covid-19 provided written informed consent to participate in our study available with the full text of this letter at NEJM.org). After Covid-19 was confirmed with a positive nasopharyngeal swab specimen at hospital admission, we obtained additional samples from the patients during hospitalization. We tested saliva specimens collected by the patients themselves and nasopharyngeal swabs collected from the patients at the same time point by health care workers. Using primer sequences from the Centers for Disease Control and Prevention, we detected more SARS-CoV-2 RNA copies in the saliva specimens (mean log copies per milliliter, 5.58; 95% confidence interval [CI], 5.09 to 6.07) than in the nasopharyngeal swab specimens (mean log copies per milliliter, 4.93; 95% CI, 4.53 to 5.33). In addition, a higher percentage of saliva samples than nasopharyngeal swab samples were positive up to 10 days after the Covid-19 diagnosis. At 1 to 5 days after diagnosis, 81% (95% CI, 71 to 96) of the saliva samples were positive, as compared with 71% (95% CI, 67 to 94) of the nasopharyngeal swab specimens. These findings suggest that saliva specimens and nasopharyngeal swab specimens have at least similar sensitivity in the detection of SARS-CoV-2 during the course of hospitalization... Published in New England J. Medicine (August 28, 2020): https://doi.org/10.1056/NEJMc2016359
|

|
Scooped by
Juan Lama
|
In 731 persons seeking COVID-19 testing at a walk-up San Francisco community site in January 2022, simultaneous nasal rapid antigen testing (BinaxNOW(TM)) and RT-PCR testing was performed. There were 296 (40.5%) positive tests by RT-PCR; 98.5% of a random sample (N=67) were the omicron variant. Sensitivity of a single antigen test was 95.2% (95% CI 92-98%); 82.1% (95% CI 77-87%) and 65.2% (95% CI 60-71%) for Ct threshold of < 30, < 35 and no threshold, respectively. We also compared BinaxNOW(TM) to RT-PCR from oral cheek swabs to nasal swabs (N=75); oral cheek specimen was significantly less sensitive than nasal swab. A single BinaxNOW(TM) oral cheek rapid antigen test failed to detect 91% (20 of 22) of specimens that were BinaxNOW(TM) positive from the standard nasal sampling. In a separate direct comparison of BinaxNOW(TM) between specimens collected from nasal or throat (tonsillar) swab (N=115), sensitivity was 97.7% for nasal and 48.8% for throat swabs that were PCR-positive on nasal swab with a Ct threshold < 30. Among persons with either a nasal or throat RT-PCR positive swab with Ct<30, BinaxNOW(TM) sensitivity was 85.7% for nasal and 89.8% for nasal plus throat swabs. BinaxNOW continues to be a very useful diagnostic during the omicron surge; oral (throat or cheek swab) should not replace nasal swabs due to significantly reduced sensitivity compared to nasal. As currently recommended, repeat testing should be done for high-risk persons with an initial negative antigen test result. Preprint available in medRxiv (Jan. 19, 2022): https://doi.org/10.1101/2022.01.08.22268954

|
Scooped by
Juan Lama
|
Researchers hope as well as preventing disease the immunisation will, crucially, stop transmission of the virus. Spanish scientists are preparing to start clinical trials of a Covid-19 vaccine nasal spray that they say could stop the spread of the virus as well as prevent people from falling ill. The vaccines that are currently available or close to approval, including the leading Pfizer/BioNTech jab, are all administered via injection, and while they are effective at preventing disease in someone who is infected with the virus, it is not yet clear if they stop people transmitting it. The Spanish team is one of a handful across the world working on nasal sprays as a means of delivering a vaccine. The theory is that inhalable vaccines activate the local immune response in the nose, mouth and throat and therefore stem infection here, making it less likely for people to pass the virus on. The vaccine would also deliver the wider systemic immunity that is delivered by any other candidate, the scientists say. A team in China submitted approval for trials of a similar nasal spray vaccine in the autumn, and the team from Spain's CSIC national research council plan to begin human trials early next year. Dr Luis Enjuanes, a virologist at the CSIC who has been studying coronaviruses for the past 40 years, told the Telegraph: "Where do we need the protection most? The virus is largely transmitted by us breathing in aerosols." Other leading experts said nasal sprays were a promising option. "If you stick a needle into an arm and go straight into tissue you activate a whole different set of cells than if you inhale a vaccine through the nose,” said Deborah Dunn-Walters, professor of immunology at the University of Surrey and a spokesperson for the British Society for Immunology. "With a respiratory virus you have the nose, mouth and lungs which have mucosal surfaces and that's how the virus gets in. To stop the virus from getting to your cells you want the antibodies at the point at which it's meeting your cells so you can block it," she said. Dr Enjuanes said his inhalable vaccine creates “a sterilising immunity, meaning there is no possibility for the virus to replicate”. Dr Enjuanes believes that the unique process his team is using will make their product “the most powerful”, claiming that the single-dose spray will offer “100 per cent protection” and pointing to good results so far in tests on mice. However, it will take time to get it to the market, he said. “Because our system is completely new, the regulatory agencies will be asking for many more controls. That’s the reason we’ll be a little bit later, assuming we are lucky and there are no negative side-effects when we start testing on humans,” said Dr Enjuanes.

|
Scooped by
Juan Lama
|
China on Wednesday approved the first phase of human testing for a nasal spray vaccine, the first trial vaccine for the coronavirus that does not require a needle injection. The spray vaccine was co-developed by researchers at Xiamen University and Hong Kong University with the aid of vaccine maker Beijing Wantai Biological Pharmacy Enterprise, Bloomberg reported. Previously, the intranasal spray method has been used to administer flu vaccines for people seeking an alternative to injections. The latest vaccine marks the 10th candidate from China to enter human trials. The announcement comes as the U.K.-headquartered company AstraZeneca was forced to pause late-stage human trials of a potential coronavirus vaccine after a spinal cord illness was detected in a patient who received the shot. Advanced Chinese vaccine developers such as CanSino Biologics and state-operated China National Biotec Group have reassured their product's efficacy amid setbacks experienced by AstraZeneca. CanSino said its shot has been safe in trials and has not caused severe side effects. An obstacle CanSino faces, however, is getting other nations to allow trials abroad. Critics are skeptical about the Chinese-made vaccine because it allegedly triggers fewer antibodies than other products currently under trial analysis, Reuters reported. Zhu Tao, CanSino's co-founder and chief scientific officer, defended the company's vaccine against criticism, saying last week that the variation in antibody readings was due to different measuring methods.

|
Scooped by
Juan Lama
|
Nasal delivery produces more widespread immune response than intramuscular injection. Scientists at Washington University School of Medicine in St. Louis have developed a vaccine that targets the SARS-CoV-2 virus, can be given in one dose via the nose and is effective in preventing infection in mice susceptible to the novel coronavirus. The investigators next plan to test the vaccine in nonhuman primates and humans to see if it is safe and effective in preventing COVID-19 infection. The study is available online in the journal Cell. Unlike other COVID-19 vaccines in development, this one is delivered via the nose, often the initial site of infection. In the new study, the researchers found that the nasal delivery route created a strong immune response throughout the body, but it was particularly effective in the nose and respiratory tract, preventing the infection from taking hold in the body. “We were happily surprised to see a strong immune response in the cells of the inner lining of the nose and upper airway — and a profound protection from infection with this virus,” said senior author Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine and a professor of molecular microbiology, and of pathology and immunology. “These mice were well protected from disease. And in some of the mice, we saw evidence of sterilizing immunity, where there is no sign of infection whatsoever after the mouse is challenged with the virus.” To develop the vaccine, the researchers inserted the virus’ spike protein, which coronavirus uses to invade cells, inside another virus – called an adenovirus – that causes the common cold. But the scientists tweaked the adenovirus, rendering it unable to cause illness. The harmless adenovirus carries the spike protein into the nose, enabling the body to mount an immune defense against the SARS-CoV-2 virus without becoming sick. In another innovation beyond nasal delivery, the new vaccine incorporates two mutations into the spike protein that stabilize it in a specific shape that is most conducive to forming antibodies against it. “Adenoviruses are the basis for many investigational vaccines for COVID-19 and other infectious diseases, such as Ebola virus and tuberculosis, and they have good safety and efficacy records, but not much research has been done with nasal delivery of these vaccines,” said co-senior author David T. Curiel, MD, PhD, the Distinguished Professor of Radiation Oncology. “All of the other adenovirus vaccines in development for COVID-19 are delivered by injection into the arm or thigh muscle. The nose is a novel route, so our results are surprising and promising. It’s also important that a single dose produced such a robust immune response. Vaccines that require two doses for full protection are less effective because some people, for various reasons, never receive the second dose.” Although there is an influenza vaccine called FluMist that is delivered through the nose, it uses a weakened form of the live influenza virus and can’t be administered to certain groups, including those whose immune systems are compromised by illnesses such as cancer, HIV and diabetes. In contrast, the new COVID-19 intranasal vaccine in this study does not use a live virus capable of replication, presumably making it safer. The researchers compared this vaccine administered to the mice in two ways — in the nose and through intramuscular injection. While the injection induced an immune response that prevented pneumonia, it did not prevent infection in the nose and lungs. Such a vaccine might reduce the severity of COVID-19, but it would not totally block infection or prevent infected individuals from spreading the virus. In contrast, the nasal delivery route prevented infection in both the upper and lower respiratory tract — the nose and lungs — suggesting that vaccinated individuals would not spread the virus or develop infections elsewhere in the body. The researchers said the study is promising but cautioned that the vaccine so far has only been studied in mice. “We will soon begin a study to test this intranasal vaccine in nonhuman primates with a plan to move into human clinical trials as quickly as we can,” Diamond said. “We’re optimistic, but this needs to continue going through the proper evaluation pipelines. In these mouse models, the vaccine is highly protective. We’re looking forward to beginning the next round of studies and ultimately testing it in people to see if we can induce the type of protective immunity that we think not only will prevent infection but also curb pandemic transmission of this virus.” Study Published in Cell (August 19, 2020): https://doi.org/10.1016/j.cell.2020.08.026
|




 Your new post is loading...
Your new post is loading...