Your new post is loading...

|
Scooped by
Juan Lama
|
The pause of use of the Moderna COVID-19 vaccine in Sweden will be extended beyond the initial December 1 end date, health officials announced. Unpublished data links the jab to heart inflammation. Swedish health officials are extending the pause of Moderna's COVID-19 vaccine in young people over continued concerns that the shot causes rare heart inflammation cases. The pause was initially supposed to last until December 1, but will now last beyond that to a date that is yet to be announced. Sweden is one of four Nordic nations that restricted the use of the jab in young people this month, with a fifth, Norway, also discouraging younger males from getting the Moderna shot. Despite the concerns arising about the vaccine in Europe, the U.S. Food and Drug Administration (FDA) has stood by its authorization of the shots, and even authorized booster shots of the vaccine earlier this week. Sweden paused usage of the Moderna COVID-19 shot in everyone born after 1990 earlier this month. The decision came after health officials viewed data that found the shots were causing cases of myocarditis in young people who got the vaccine. Sweden's Public Health Agency says that the unpublished data signals 'an increased risk of side effects such as inflammation of the heart muscle or the pericardium' - the double-walled sac containing the heart and the roots of the main vessels. It added: 'The risk of being affected is very small.' That data is still not publicly available. Denmark followed Sweden's lead, and restricted access to the vaccine to anyone under the age of 18 as well. The Finnish Institute for Health and Welfare said earlier this month that authorities won't give the vaccine to males under age 30, and they will be offered the Pfizer-BioNTech immunization instead, also citing the heart inflammation data. Iceland also paused use of the vaccine citing concerns from the same data. Norway, another Nordic country, has not taken as drastic action as its neighbors, with health officials urging people under 30 to opt for the Pfizer vaccine instead. Heart inflammation is also a symptom of many viral infections like COVID-19, though, and the likelihood of developing the inflammation after infection is much higher than it is after vaccination. Those conditions involve an inflammation of the heart or its lining. On Thursday, data on the Moderna vaccines likelihood to cause heart inflammation was presented to a CDC advisory panel. The presentation showed that males were much more likely to develop the condition than females - with those aged 18 to 24 at most risk, and the 25 to 29 group at risk as well. The second dose of the vaccine is also the one that usually causes the condition. Myocarditis risk falls off after age 30, though. The data also shows that people who receive the Moderna shot are more likely to develop myocarditis. For every one million doses of the Moderna shot administered, there are 13.3 more cases of myocarditis detected compared to every one million of the Pfizer jab. The reason for this is now yet known. The increased risk seems to appear for both males and females. 'The connection is especially clear when it comes to Moderna's vaccine Spikevax, especially after the second dose,' the Swedish health agency said. A Moderna spokesperson said in an email last week that the company was aware of the decisions by regulators in Denmark and Sweden to pause the use of its vaccine in younger individuals because of the rare risk of myocarditis and or pericarditis. 'These are typically mild cases and individuals tend to recover within a short time following standard treatment and rest,' they wrote. 'The risk of myocarditis is substantially increased for those who contract COVID-19, and vaccination is the best way to protect against this.' According to one U.S. study that has yet to undergo peer review, young males under agr 20 are up to six times more likely to develop myocarditis after contracting COVID-19 than those who have been vaccinated. Denmark said that, while it used the Pfizer vaccine as its main option for people aged 12 to 17 years, it had decided to pause giving the Moderna vaccine to people below 18 according to a 'precautionary principle'. In June, the CDC issued a warning that young males were at an increased risk of myocarditis after receiving the vaccine. The label for both the Pfizer and Moderna vaccines were changed in the U.S. to reflect the warning, though usage was never paused. Cases of inflammation after vaccination are rare, though they do occur often enough to concern regulators. A recent study from Kaiser Permanente Southern California found that around seven out of every one million people that receive a two-shot COVID-19 vaccine will develop myocarditis. The same study found that 47.5 out of every one million Covid patients experience heart inflammation. While myocarditis will often resolve itself, it can be dangerous. Heart inflammation can often lead to fatigue, shortness of breath and chest pain for patients. People with inflamed hearts are at a higher risk for heart failure, heart attacks and strokes. Attempting strenuous physical activity with an inflamed heart could also potentially lead to sudden cardiac arrest, or even death.

|
Scooped by
Juan Lama
|
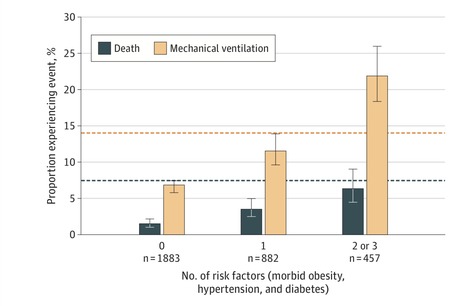
This case series examines the clinical outcomes for young adults hospitalized with COVID-19. Young adults age 18 to 34 years hospitalized with COVID-19 experienced substantial rates of adverse outcomes: 21% required intensive care, 10% required mechanical ventilation, and 2.7% died. This in-hospital mortality rate is lower than that reported for older adults with COVID-19, but approximately double that of young adults with acute myocardial infarction. Morbid obesity, hypertension, and diabetes were common and associated with greater risks of adverse events. Young adults with more than 1 of these conditions faced risks comparable with those observed in middle-aged adults without them. More than half of these patients requiring hospitalization were Black or Hispanic, consistent with prior findings of disproportionate illness severity in these demographic groups. Published in JAMA (Sept. 9, 2020): https://doi.org/10.1001/jamainternmed.2020.5313

|
Scooped by
Juan Lama
|
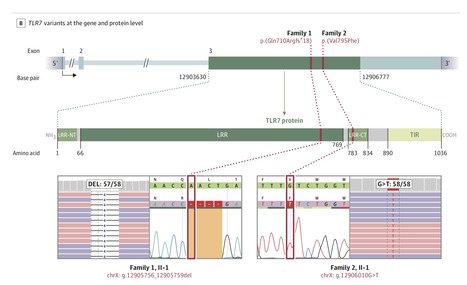
This case series describes rare putative X-chromosomal loss-of-function variants associated with impaired peripheral mononuclear blood cell interferon signaling in 4 young male patients hospitalized with severe coronavirus disease 2019 (COVID-19) in the Netherlands. Severe coronavirus disease 2019 (COVID-19) can occur in younger, predominantly male, patients without preexisting medical conditions. Some individuals may have primary immunodeficiencies that predispose to severe infections caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). To explore the presence of genetic variants associated with primary immunodeficiencies among young patients with COVID-19. Case series of pairs of brothers without medical history meeting the selection criteria of young (age <35 years) brother pairs admitted to the intensive care unit (ICU) due to severe COVID-19. Four men from 2 unrelated families were admitted to the ICUs of 4 hospitals in the Netherlands between March 23 and April 12, 2020. The final date of follow-up was May 16, 2020. Available family members were included for genetic variant segregation analysis and as controls for functional experiments. Results of rapid clinical whole-exome sequencing, performed to identify a potential monogenic cause. Subsequently, basic genetic and immunological tests were performed in primary immune cells isolated from the patients and family members to characterize any immune defects. The 4 male patients had a mean age of 26 years (range, 21-32), with no history of major chronic disease. They were previously well before developing respiratory insufficiency due to severe COVID-19, requiring mechanical ventilation in the ICU. The mean duration of ventilatory support was 10 days (range, 9-11); the mean duration of ICU stay was 13 days (range, 10-16). One patient died. Rapid clinical whole-exome sequencing of the patients and segregation in available family members identified loss-of-function variants of the X-chromosomal TLR7. In members of family 1, a maternally inherited 4-nucleotide deletion was identified (c.2129_2132del; p.[Gln710Argfs*18]); the affected members of family 2 carried a missense variant (c.2383G>T; p.[Val795Phe]). In primary peripheral blood mononuclear cells from the patients, downstream type I interferon (IFN) signaling was transcriptionally downregulated, as measured by significantly decreased mRNA expression of IRF7, IFNB1, and ISG15 on stimulation with the TLR7 agonist imiquimod as compared with family members and controls. The production of IFN-γ, a type II IFN, was decreased in patients in response to stimulation with imiquimod. In this case series of 4 young male patients with severe COVID-19, rare putative loss-of-function variants of X-chromosomal TLR7 were identified that were associated with impaired type I and II IFN responses. These preliminary findings provide insights into the pathogenesis of COVID-19. Published in JAMA (July 24, 2020): https://doi.org/10.1001/jama.2020.13719
|

|
Scooped by
Juan Lama
|
Although antibodies induced by SARS-CoV-2 infection are largely protective, they do not completely protect against reinfection in young people, as evidenced through a longitudinal, prospective study of more than 3,000 young, healthy members of the US Marines Corps conducted by researchers at the Icahn School of Medicine at Mount Sinai and the Naval Medical Research Center, published April 15 in The Lancet Respiratory Medicine. "Our findings indicate that reinfection by SARS-CoV-2 in health young adults is common" says Stuart Sealfon, MD, the Sara B. and Seth M. Glickenhaus Professor of Neurology at the Icahn School of Medicine at Mount Sinai and senior author of the paper. "Despite a prior COVID-19 infection, young people can catch the virus again and may still transmit it to others. This is an important point to know and remember as vaccine rollouts continue. Young people should get the vaccine whenever possible, since vaccination is necessary to boost immune responses, prevent reinfection, and reduce transmission." The study, conducted between May and November 2020, revealed that around 10 percent (19 out of 189) of participants who were previously infected with SARS-CoV-s (seropositive) became reinfected, compared with new infections in 50 percent (1.079 out of 2,247) of participants who had not been previously infected (seronegative). While seronegative study participants had a five times greater risk of infection than seropositive participants, the study showed that seropositive people are still at risk of reinfection. The study population consisted of 3,249 predominantly male, 18-20-year-old Marine recruits who, upon arrival at a Marine-supervised two-week quarantine prior to entering basic training, were assessed for baseline SARS-CoV-2 IgG seropositivity (defined as a 1:150 dilution or greater on receptor binding domain and full-length spike protein enzyme-linked immunosorbent [ELISA] assays.) The presence of SARS-CoV-2 was assessed by PCR at initiation, middle and end of quarantine. After appropriate exclusions, including participants with a positive PCR during quarantine, the study team performed three bi-weekly PCR tests in both seronegative and seropositive groups once recruits left quarantine and entered basic training. Recruits who tested positive for a new second COVID-19 infection during the study were isolated and the study team followed up with additional testing. Levels of neutralising antibodies were also taken from subsequently infected seropositive and selected seropositive participants who were not reinfected during the study period. Of the 2,346 Marines followed long enough for this analysis of reinfection rate, 189 were seropositive and 2,247 were seronegative at the start of the study. Across both groups of recruits, there were 1,098 (45%) new infections during the study. Among the seropositive participants, 19 (10%) tested positive for a second infection during the study. Of the recruits who were seronegative, 1,079 (48%) became infected during the study. To understand why these reinfections occurred, the authors studied the reinfected and not infected participants' antibody responses. They found that, among the seropositive group, participants who became reinfected had lower antibody levels against the SARS-CoV-2 virus than those who did not become reinfected. In addition, in the seropositive group, neutralising antibodies were less common (neutralising antibodies were detected in 45 (83%) of 54 uninfected, and in six (32%) of 19 reinfected participants during the six weeks of observation). Comparing new infections between seropositive and seronegative participants, the authors found that viral load (the amount of measurable SARS-CoV-2 virus) in reinfected seropositive recruits was on average only 10 times lower than in infected seronegative participants, which could mean that some reinfected individuals could still have a capacity to transmit infection. The authors note that this will need further investigation. In the study, most new COVID-19 cases were asymptomatic—84% (16 out of 19 participants) in the seropositive group vs 68% (732 out of 1,079 participants) in the seronegative group—or had mild symptoms and none were hospitalised. The authors note some limitations to their study, including that it likely underestimates the risk of reinfection in previously infected individuals because it does not account for people with very love antibody levels following their past infection. They strongly suggest that even young people with previous SARS-CoV-2 infection be a target of vaccination since efforts must be made to prevent transmission and prevent infection amongst this group. Study cited was published in The Lancet Respiratory Medicine (April 15, 2021): https://doi.org/10.1016/S2213-2600(21)00158-2

|
Scooped by
Juan Lama
|
A Stanford University report shows that teens and young adults who use e-cigarettes are five to seven times more likely to test positive for the virus. Since the pandemic started to hit the US in full force in March, speculation about the link between vaping and Covid-19 has flourished. The Food and Drug Administration and the National Institute on Drug Abuse both issued warnings. Anecdotal reports of young vapers coming down with severe coronavirus infections began to crop up. But there was very little research to support a connection. Now, a study published today in The Journal of Adolescent Health finally offers data that shows a relationship between e-cigarette use and Covid-19 risk. Researchers from Stanford University show that teenagers and young adults ages 13 to 24 who use e-cigarettes are five times more likely to be diagnosed with Covid-19 than their non-vaping peers. Those who are dual users—people who smoke both traditional and electronic cigarettes—are seven times more likely to test positive for the virus, the researchers found. “I knew there would be a relationship,” says coauthor Bonnie Halpern-Felsher, a professor of pediatrics at Stanford University who studies youth tobacco use. “I did not expect it to be this strong of a relationship.” Studies have already linked smoking with higher susceptibility to severe Covid-19 infections, but previously no population-based studies had examined the link between e-cigarette use and Covid-19 in teenagers and young adults. The question researchers wanted to answer was two-fold: Were e-cigarette smokers more likely to get tested for SARS-CoV-2? And were they more likely to test positive? “The answer is soundly yes” to both parts of the question, says Halpern-Felsher. The researchers gathered their data through an online survey posted on spaces like social media and gaming sites. Over 4,000 teens and young adults from all 50 states responded, completing the roughly 15-minute survey. Researchers then weighted the samples to reflect the racial and ethnic, gender, LGBTQ status, and age makeup of the United States population. The survey, which was sent out in early May, asked respondents whether they had ever used regular or electronic cigarettes; whether they had used them in the last 30 days; whether they had been tested for Covid-19; and whether their test results came back positive. The researchers also controlled for other Covid-19 risk factors like whether the respondents lived near a coronavirus hotspot; whether they were under- or overweight, which can affect lung function; and for their socio-economic status, which can affect how well people can socially distance. Ultimately, the researchers determined that dual users who had smoked in the last 30 days were not only more likely to test positive, but they were also nine times more likely to get tested in the first place. The survey did not explore why users decided to get tested. It’s possible that users confused the effects of vaping—extra phlegm, coughing, or shortness of breath—with Covid-19 symptoms. But the high rate of positive test results may indicate that vapers are more vulnerable to the virus itself. That said, this study simply illustrates a correlation between e-cigarette and cigarette use and positive Covid-19 diagnoses. As the authors explain in the paper, their findings “show that e-cigarette use and dual use of e-cigarettes and cigarettes are significant underlying risk factors for COVID-19 that has previously not been shown.” But on its own, this paper can’t prove whether they may be more biologically susceptible to infection in the first place, or if they are more likely to have severe infections. Still, Halpern-Felsher has a few theories for why this overlap might exist. Smokers may have more lung damage, making them more susceptible to the virus. Or they might be touching their hand to their mouth more often than other people, or sharing vapes, increasing their likelihood of being exposed in the first place. Or it could be that the virus is being spread through the aerosols vapers exhale. “Those are all hypotheses,” she says. “Someone needs to follow it up.” There are already studies that link smoking tobacco with a higher risk of Covid-19. A study published in March in the European Respiratory Journal found that smokers and those with chronic obstructive pulmonary disease had greater expression of ACE2, the protein SARS-CoV-2 uses to enter cells. In a meta-analysis of 19-papers published in May in the journal Nicotine and Tobacco Research, scientists from UC San Francisco found that tobacco use nearly doubled a person’s risk of severe Covid-19 infection. Another study by a separate group of researchers at UCSF published in the Journal of Adolescent Health in July found that smoking also doubled the risk of Covid-19 infection for young adult ages 18 to 25. Original study published in the Journal of Adolescent Health (August 11, 2020):
|



 Your new post is loading...
Your new post is loading...